Understanding Angioplasty: What Every Patient Should Know
Angioplasty is one of the most common and effective procedures in interventional cardiology. As someone who has performed hundreds of these procedures, I want to help you understand what angioplasty involves, when it’s needed, and what you can expect during the process.
What is Angioplasty?
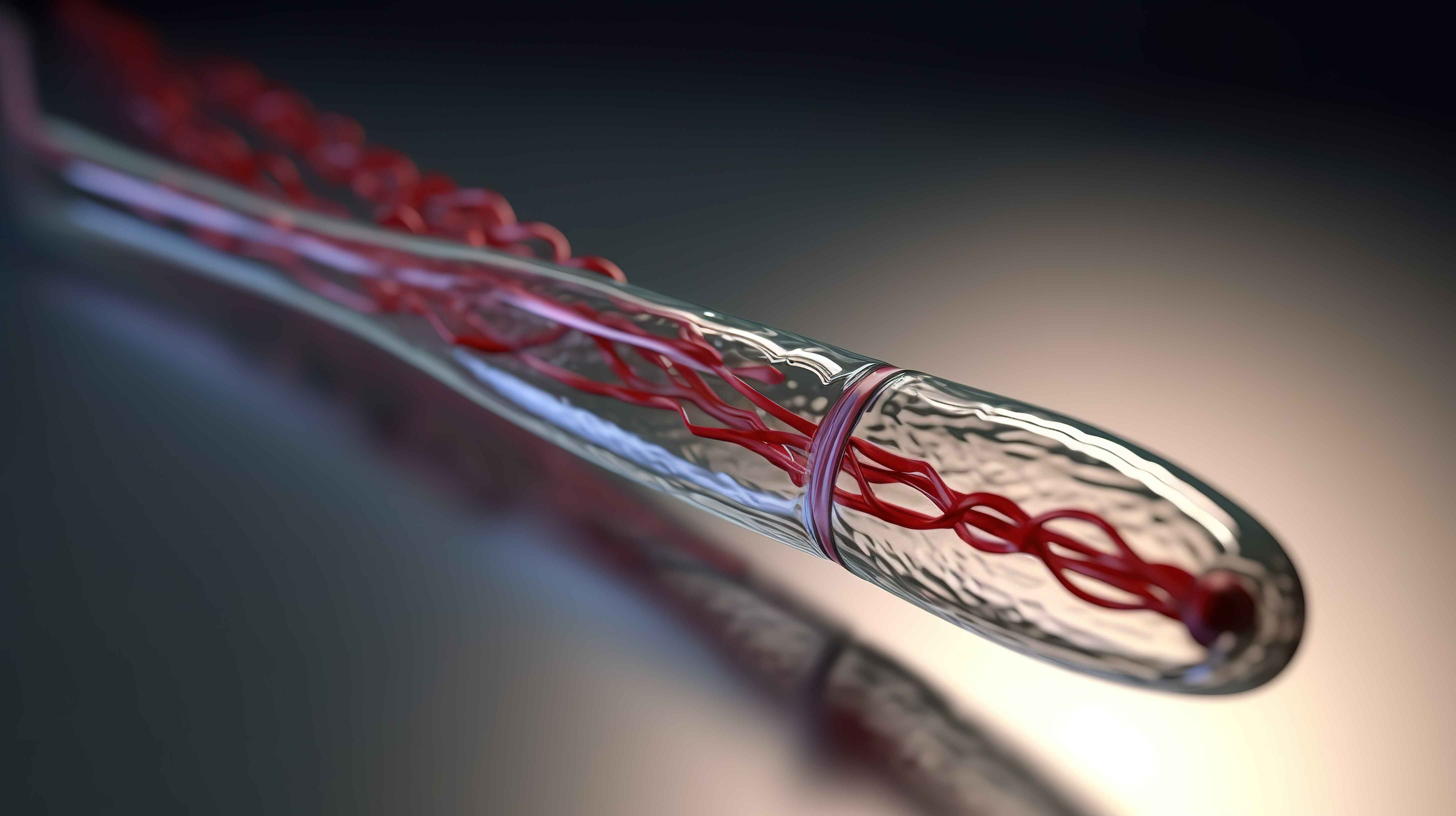
Angioplasty, also known as Percutaneous Coronary Intervention (PCI), is a minimally invasive procedure used to open blocked or narrowed coronary arteries. The procedure involves inserting a small balloon into the blocked artery and inflating it to compress the plaque against the artery walls, restoring blood flow to the heart muscle.
When is Angioplasty Recommended?
Your cardiologist may recommend angioplasty if you have:
Acute Conditions
- Heart attack (ST-elevation myocardial infarction)
- Unstable angina with high-risk features
- Cardiogenic shock
Chronic Conditions
- Stable angina that doesn’t respond to medication
- Significant coronary artery disease affecting daily activities
- Failed medical therapy for coronary artery disease
Types of Angioplasty
1. Balloon Angioplasty
- Simple balloon inflation to compress plaque
- Rarely used alone in modern practice
- Risk of artery re-narrowing (restenosis)
2. Stent Angioplasty
- Bare Metal Stents (BMS): Metal scaffolding to keep artery open
- Drug-Eluting Stents (DES): Coated with medication to prevent restenosis
- Bioresorbable Stents: Dissolve over time (newer technology)
The Angioplasty Procedure: Step by Step
Before the Procedure
- Pre-procedure assessment: Blood tests, ECG, chest X-ray
- Medication review: Adjustments to current medications
- Consent process: Discussion of risks and benefits
- Preparation: Fasting, IV line insertion, pre-medication
During the Procedure
- Access: Usually through the wrist (radial) or groin (femoral) artery
- Catheter insertion: Thin tube guided to the heart
- Contrast injection: To visualize the blocked artery
- Balloon inflation: To compress the plaque
- Stent placement: If required (in most cases)
- Final assessment: Ensure good blood flow restoration
After the Procedure
- Monitoring: In the catheterization lab recovery area
- Observation: Typically 4-6 hours for radial access, longer for femoral
- Medication: Antiplatelet drugs to prevent clot formation
What to Expect: Recovery Timeline
First 24 Hours
- Rest: Limited activity, bed rest initially
- Monitoring: Heart rhythm, blood pressure, access site
- Hydration: Important for contrast dye elimination
First Week
- Gradual activity increase: Short walks, light daily activities
- Access site care: Keep clean and dry, watch for complications
- Medication adherence: Critical for preventing complications
First Month
- Cardiac rehabilitation: May be recommended
- Follow-up appointments: With your cardiologist
- Lifestyle modifications: Diet, exercise, smoking cessation
Potential Risks and Complications
While angioplasty is generally safe, potential risks include:
Common (< 5%)
- Bleeding at access site
- Bruising or hematoma
- Temporary kidney dysfunction from contrast dye
Rare (< 1%)
- Heart attack during procedure
- Stroke
- Emergency bypass surgery
- Allergic reaction to contrast
- Artery perforation
Success Rates and Long-term Outcomes
Immediate Success
- Technical success: > 95% of cases
- Symptom relief: Most patients experience immediate improvement
- Blood flow restoration: Typically excellent
Long-term Results
- Stent patency: 90-95% at 1 year with drug-eluting stents
- Symptom control: Significant improvement in quality of life
- Survival benefit: Especially in acute heart attacks
Post-Angioplasty Medications
Antiplatelet Therapy
- Aspirin: Lifelong (usually 81mg daily)
- P2Y12 inhibitor: Clopidogrel, Prasugrel, or Ticagrelor for 6-12 months
Other Medications
- Statins: For cholesterol management
- ACE inhibitors or ARBs: For blood pressure and heart protection
- Beta-blockers: If indicated
Lifestyle Changes for Success
Diet Modifications
- Mediterranean-style diet
- Reduce sodium intake (< 2300mg daily)
- Limit saturated fats
- Increase fiber intake
Physical Activity
- Cardiac rehabilitation program
- Gradual exercise progression
- Regular moderate exercise (150 minutes weekly)
Risk Factor Management
- Smoking cessation (absolute must)
- Diabetes control (HbA1c < 7%)
- Blood pressure control (< 130/80 mmHg)
- Stress management
When to Seek Immediate Medical Attention
Contact emergency services or your cardiologist immediately if you experience:
- Chest pain similar to or worse than before
- Shortness of breath at rest
- Excessive bleeding from access site
- Numbness or weakness in arms or legs
- Severe headache or vision changes
Frequently Asked Questions
Q: How long does the procedure take?
A: Typically 30-60 minutes, depending on complexity.
Q: Will I need repeat procedures?
A: Modern drug-eluting stents have low restenosis rates (5-10%).
Q: Can I drive after angioplasty?
A: Usually after 1 week if no complications, but consult your doctor.
Q: Will I feel the stent?
A: No, you won’t feel the stent once it’s placed.
Conclusion
Angioplasty is a highly effective treatment for coronary artery disease that can dramatically improve your quality of life and, in many cases, save your life. The key to long-term success lies not just in the procedure itself, but in your commitment to lifestyle changes and medication adherence afterward.
Remember, angioplasty treats the symptom (blocked artery) but doesn’t cure the underlying disease (atherosclerosis). Continued medical care and lifestyle modifications are essential for preventing future problems.
Dr. Mohsin Bilal is a consultant cardiologist and interventional cardiologist at Avanti Hospital Ujjain. He has performed over 1000 angioplasty procedures and specializes in complex coronary interventions.
Concerned about chest pain or need an angioplasty consultation? Schedule an appointment with Dr. Mohsin Bilal today.
Need Professional Cardiac Care?
Schedule a consultation with Dr. Mohsin Bilal for personalized heart health advice.